“It is curable!!” yes most of the brain tumor can now be safely and successfully treated with modern day surgical techniques. Find out more about our dept. of brain tumor…….
At Jaslok Hospital in Mumbai, we understand the profound impact a brain tumor can have on a person’s life and the lives of their loved ones. As one of the leading medical institutions in India, we take immense pride in providing top-notch healthcare services, especially in the field of neurosurgery and brain tumor treatment in Mumbai. Our team of highly qualified, skilled doctors and healthcare professionals are dedicated to offering personalized care and cutting-edge treatments to ensure the best possible outcomes for our patients. brain tumor kya hota h
Brain tumors are known to be notorious and dreaded ailment among human being since ancient period. Ancient literature shows that this entity was known then but most of these tumors were diagnosed at post-mortem. The situation remained same till 20 th century when development of imaging and other diagnostic modalities helped us to know much about brain tumors, its diagnosis and timely intervention. Till date, a lot of research work has been done over brain tumor to know its pathogenesis, genetic causes and targeted therapies but still many questions are unanswered. Most important part is that despite of advances in
treatment modalities, brain tumor remains one of the dangerous illnesses in terms of both mortality and morbidity.
Brain tumors can be divided into primary and secondary. Primary brain tumors arise in brain itself while secondary tumors are metastasis from malignancies of other body parts. Primary brain tumors are rare as compared to other cancers of body. Although it constitutes about 1 – 2% of total cancers but is responsible for about 20% deaths due to cancer related causes. In India, the incidence is about 2/10000 people. Primary brain tumors are both benign and malignant. About 33% of primary brain tumors are malignant. No age group is spared from brain tumors. It affects all from pediatric age group to elderly patients. The incidence among various age groups is different according to type of tumor. Sex ratio is also variable according to type of tumors. In nutshell, no age group or sex is immune to brain tumors.
Previously brain tumors were classified according to histogenesis and similarities with different putative cells of origin and their presumed level of differentiation (WHO classification 2007) like glioma, meningioma, pituitary tumor, medulloblastoma, ependymoma, chordoma etc. But latest WHO classification 2016 breaks the principle of diagnosis based only on microscopy and incorporates the molecular parameters in classification.
A brain tumor is an uncontrolled and abnormal rapid growth of cells in the brain. These tumors can be either benign (non-cancerous) or malignant (cancerous). They may originate from the brain cells/tissue itself or spread from other parts of the body.
Understanding the diverse types of brain tumors is of utmost importance for accurate diagnosis and determining the most suitable treatment options.
Gliomas are the most prevalent type, arising from glial cells of the brain that support and nourish nerve cells. This family includes different variations:
These tumors originate from astrocytes, a specific type of glial cell. They can be either slow-growing (low-grade) or fast-growing and malignant (high-grade), with high-grade astrocytomas like glioblastomas being particularly aggressive, high recurrence rate and challenging to treat with guarded prognosis.
Forming from oligodendrocytes, another type of glial cell, oligodendrogliomas are relatively uncommon and may have a slower growth rate compared to some other gliomas. They are less aggressive then high grade gliomas in nature and recurrence.
Representing the most severe and aggressive form of gliomas, glioblastomas grow more rapidly and are associated with a poor prognosis.
Developing in the meninges, the protective layers surrounding the brain and spinal cord, most meningiomas are benign, but some can be more aggressive and challenging to treat.
Emerging within the pituitary gland at the base of the brain, pituitary tumors can disrupt hormonal regulation of the body and often require specialized treatment, in the form or surgical and medical with hormonal therapy.
Fast-growing, high-grade tumors commonly found in the cerebellum, particularly in children, may interferes with child’s normal development which necessitates its early diagnosis and treatment for better outcomes.
Chordomas are soft, slow-growing tumors that typically arise from the bones, occur at the base of the skull or along the spine, posing treatment challenges and necessitating a comprehensive approach due to its unusual location
Hemangioblastomas are rare, benign tumors that can occur in the brain and spinal cord, often associated with Von Hippel-Lindau (VHL) disease, which is a genetic chromosomal disorder. VHL is also associated with other abnormalities in body along with hemangioblastomas.
Originating from Schwann cells associated with nerve fibers, schwannomas are usually benign and often occur on nerves related to hearing (vestibular schwannoma). They have a very slow growth rate, but once it disrupts the hearing, it will be permanent.
Pineal region tumors, including pineal parenchymal tumors and germ cell tumors, develop in or near the pineal gland (centre of the brain), affecting functions like hormone regulation and sleep-wake cycles. Can occur in any age group from childhood to late elderly age.
Typically found near the pituitary gland, craniopharyngiomas can cause complications due to their location. They are usually benign but can significantly affect nearby structures, and interference with vision and hormonal disturbances in body.
Developed from the ependymal lining of the ventricles or the spinal canal, ependymomas can be slow-growing (low-grade) or more aggressive (high-grade), requiring careful evaluation for appropriate treatment planning.
Brain tumor symptoms can vary depending on the tumor’s location, size, and rate of growth. Some common symptoms include:
Persistent and severe headaches that may worsen over time, especially in the morning.
Uncontrolled electrical disturbances in the brain which can cause fits, convulsions or blackouts.
Weakness, numbness, or tingling in the limbs, difficulty in balancing, or problems with vision and speech.
Memory problems, confusion, and changes in concentration and decision-making abilities. Vomitings: due to increase in intracranial pressure. Brain tumor ke lakshan
The exact causes of brain tumors remain largely unknown, but certain risk factors may increase their likelihood, such as:
At Jaslok Hospital, we offer a wide range of advanced treatment options for brain tumors. Our team of neurosurgeons, oncologists, and radiation therapists work together to develop personalized treatment plans for each patient. The comprehensive treatment plan includes:
At Jaslok Hospital, we prioritize the well-being of our patients not only during treatment but also post-treatment. We provide comprehensive support services, including counseling, rehabilitation, and pain management, to ensure a smooth recovery process. Our dedicated team of healthcare professionals ensures that patients receive appropriate follow-up care to monitor their progress and address any concerns.
Jaslok Hospital has earned its reputation as the best hospital for brain tumor in Mumbai through a combination of excellence, expertise, and empathy. Our commitment to patient-centric care, coupled with cutting-edge technology and innovative treatments, sets us apart as a leading healthcare institution in the field of brain tumour treatment options.
Our team of world-class neurosurgeons and oncologists is the backbone of our success. The team is led by the best Neurosurgeon in India, Dr. Paresh K Doshi. With their extensive experience and expertise in managing complex brain tumor cases, patients can be assured of receiving the highest quality of care possible. Apart from open brain surgeries, he has expertise in stereotactic brain surgeries (minimally invasive) for tumour patients also.
At Jaslok Hospital, we understand the importance of offering non-invasive treatment options for brain tumors also. Our state-of-the-art facilities allow us to provide cutting-edge therapies, such as stereotactic radiosurgery and targeted radiation, minimizing the impact on surrounding healthy brain tissue while effectively targeting the tumor cells.
The clinic is equipped with the latest technology and state-of-the-art infrastructure to ensure precise diagnosis and effective brain tumor treatment in Mumbai. Our commitment to staying at the forefront of medical advancements enables us to provide the best possible outcomes for our patients.
The etiology of brain tumors remains unclear till date. The various etiological hypotheses are postulated from time to time but none is able to define etiopathogenesis of brain tumors completely. In recent years, a lot of work has been done over molecular basis of brain tumors. Multiple mutations, aberrations, deletions and various genetic gateways are identified and their role in the pathogenesis of brain tumors is established. Some infections like EBV are also responsible for some tumors like lymphomas. Some tumors like craniopharyngiomas, rathke’s cleft cyst, epidermoid, dermoids etc. are considered to be due to aberrant development.
Symptomatology of brain tumors is very vague and dramatic. Benign and some malignant primary tumors have gradual onset and progressive course while highly malignant tumors and metastasis presents abruptly and patient deteriorates very rapidly. Most of the symptoms are due to pressure effect of the tumor itself and presents as symptoms of raised intracranial tension. Important symptoms of brain tumors are summarized below.

These symptoms are according to the site of the tumor. These symptoms are:-
Frontal lobe:
Parietal lobe:
Temporal lobe:
Occipital lobe:
Thus the symptoms are too vague to diagnose the brain tumors only on the basis of symptoms. But these symptoms must trigger a clinician to look for any mass lesion in brain.
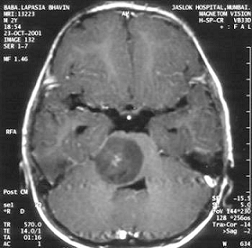
Diagnosis is made mainly by imaging (CT scan, MRI). Advent of MR spectroscopy helps a lot in differentiating benign and malignant tumors, infarcts, infection and other mass lesions. For common or new onset headaches a simple investigation would be CT scan. However, most doctors will advise MRI as the first form of diagnosis as it gives better definition of intracranial structures as compared to MRI.

Multiple risk factors are postulated though their direct role in pathogenesis of brain tumors is not fully established. The various risk factors are as:
The mainstay of the treatment of brain tumors is surgery. Other supportive therapies like chemotherapy, radiotherapy etc. helps in disease free survival. No medical management is available to treat brain tumors completely. Some drugs are used to reduce tumor edema (steroids), treat seizures and headache but have no role in treatment of tumor itself.
Surgery
It is the mainstay of treatment. The aim of surgery to remove mass effect, get tissue for histopathological diagnosis and excision of mass to cure the disease. Surgery aims at total or gross total excision, but in case of inoperable tumors (eloquent areas) near total excision or simple decompression is also done. Surgery causes immediate relief in mass effect. Benign tumors are usually cured by surgery itself but malignant tumors require chemotherapy or radiotherapy as an adjuvant. Recurrence is the rule in case of malignant brain tumors but recurrence free survival depends upon the type and grade of the tumor. Even after recurrence, surgery is the first line of management. Now a day, advances in surgical techniques facilitate more excision with less deficits and morbidity. Tractography, neuronavigation, CUSA, intraoperative MRI, flouroscine microscopy, intraoperative neurophysiological monitoring are few advances in surgical techniques which improve the result of surgery.
This is recent advance in surgery of brain tumors in which there is computerized software based mapping of tumor and its relation to various eloquent brain areas, blood vessels, tracts and neuron bundles is done. Preoperative MRI, functional MRI and DTI (Tractography) is used to prepare a 3D map of tumor with its surrounding structures. It also helps in deciding the territory through which tumor can be approached easily. Using it, we are excising the tumors which are considered inaccessible due to its location near eloquent and important structures. As a result, maximum possible reductions of tumor load with minimal or no neurodeficits is offered to the patient.

Neurophysiological monitoring:
This is also recent practice in neurological surgeries. Many tumors are located in such areas where any attempt to excision may lead to permanent neurodeficits. Intraoperative neurophysiological monitoring is real time recording of various brain activities during surgery. Even touching of important structures immediately reflects as changes in NP monitoring and those structures can be saved and deficits can be avoided. This results in safe excision of tumors.


Stereotactic Surgery:
This is new concept which uses stereotactic frame to approach the lesion without craniotomy and damaging the vital structures. The tumors which are not approachable or at eloquent areas can be approached through stereotactic surgery and tissue can be obtained for histopathological diagnosis so that further therapies can be initiated. Thus the tumors which were previously considered untreatable are now treated. For further information: read- Stereotactic Procedure

Gamma knife:
This is a type of focused radiotherapy which delivers computer software based, multiple source high dose of radiation to the small diseased area of brain without affecting surrounding brain tissue thus avoiding side effects of whole brain radiation. The tumors which are inoperable or inaccessible can be treated by gamma knife.
Chemotherapy:
This has limited role in brain tumors due to presence of blood brain barrier. Few chemotherapeutic agents like temozolamide, carmustine, CCNU, procarbazine, cytarabine, vinblastine etc. are effective against brain tumors. The modality is usually used as adjuvant to surgery.
Radiotherapy:
This is also adjuvant to surgery. As alone it has limited role but potential side effects in form of radiation necrosis.
Immunotherapy:
This is in juvenile phase. Few molecules are developed to target molecular pathology of the tumor.
Stereotactic surgery is a minimally invasive procedure. It makes use of a three-dimensional coordinate system to accurately locate small targets within the brain and subsequent procedures such as stimulation, lesioning, implantation ), ablation etc. can be performed.
Theoritically any organ inside the body can be subjected to stereotactic surgery. Difficulties in putting up a reliable frame of reference (such as bony landmarks which has a constant spatial relation to soft tissues) however, mean that its applications have been limited to brain surgery.

History of Stereotactic Surgery in India
Functional and stereotactic surgeries were first introduced in 1940’s and 50’s, but did not make progress as expected due to high mortality and morbidity rates. Neurosurgery developed in India after the II world war. In 1940 pioneers like Chintan Nambiar performed 74 cases of chemopallidotomy using free hand stereotactic technique. In 1949 Jacob Chandy and Baldev Singh established the first neurosurgical center at Christian Medical College (CMC), Vellore in Tamilnadu. In 1950’s V. Balasubramaniam and B. Ramamurthi performed pallidal lesioning with inflatable balloon and alcohol. H M Dastur started stereotactic surgery at King Edward Memorial (KEM) Hospital Mumbai in 1959. Initially he used Oliver’s guide and later used Narabayashi frame along with Dr. Gajendra Sinh (Jaslok hospital, Mumbai) to perform stereotactic surgery. Dr S N Bhagwati (Mumbai) used Mckinneys apparatus and Leksell’s frame in 1964. In 1970, S. Kalyanaraman (Madras Medical College) performed stereotactic surgeries using a combination of Leksell and Sehgal stereotactic equipment to perform simultaneous targeting of intracranial structures. R M Verma who was trained in Bristol started neurosurgical units in AIIMS and was instrumental in establishing National Institute of Mental Health and Neurosciences (NIMHANS).
The Indian Society of Stereotactic and Functional Neurosurgery were formed in 1997 with V. Balasubramaniam, as its first President. Stereotactic Radiosurgery was first introduced in India at the Apollo Hospital, Chennai using Linac X-knife system. Gamma knife was introduced at Hinduja Hospital, Mumbai in 1997. In Mumbai Dr. Paresh Doshi (Jaslok Hospital, Mumbai) performed surgery for Parkinson’s disease. Initially he started with GPi lesioning and later switched to STN-DBS surgery. In 2009 he was instrumental in performing neural transplant surgery using Mesenchymal Stem cell therapy in collaboration with Reliance Life sciences for Parkinson’s disease. The results of which are awaited.
About Stereotactic Brain Biopsy
A Stereotactic Brain Tumor Biopsy is a neurosurgical procedure in which samples of tissue are taken from the tumor site. The biopsy will provide information about the type of tumor. The purpose of a biopsy is to discover the type and grade of a tumor as well as its molecular biology and its growth pattern. With the help of MRI and CT scans and 3D computer workstations, it is possible to accurately target any area of the brain. A stereotactic biopsy surgery is the most accurate method of obtaining a diagnosis. Once a sample is obtained, a pathologist examines the tissue under a microscope and writes a pathology report containing an analysis of the brain tissue.

Indications
This procedure is used by neurosurgeons to obtain tissue samples of areas within the brain from where the sample needs to be taken. The main indications for stereotactic biopsy are lesions that are located deep within the brain, multiple lesions, lesions in candidates who cannot tolerate general anesthesia. We perform stereotactic biopsies under local anaesthesia, with or without intravenous sedation. Most of the biopsies are performed with CT localization, however, in cases where the lesion can only be seen on MRI we have facilities to do MRI guided biopsies. The procedure takes about 3 hours. To begin with a stereotactic frame is attached to the patient’s head using local anaesthesia at the pin insertion site.
In the operating room, the patient’s head is rested on a clamp system in a comfortable position. An incision of only a few millimeters is made in the scalp and a small hole is drilled into the skull. A thin biopsy needle is inserted into the brain using the coordinates obtained on the computer workstation. This is less invasive and much more precise than an open biopsy that requires a craniotomy which involves removing a piece of the skull in order to get access to the brain. The specimen is then sent to the pathologist for evaluation who will opine if the tissue is representative of the lesion and adequate for him to give final diagnosis. Patients are monitored for several hours following the procedure and usually go home within 1-2 days.
Risks –
The risks associated with stereotactic brain biopsy are minimal. The complication rate of a stereotactic brain tumor biopsy is 2.3%, predominately caused by hemorrhage (0.7%), and edema or infection (< 2%). The diagnostic accuracy is 97%. Sometimes the sample of tissue obtained may be non-diagnostic, in which case repeat biopsy is advised.
Surgery is required to decrease the pressure in the brain and to know the nature of the tumor definitively. Medicines can’t cure most of the brain tumours.
Out of all primary brain tumors (those arising in the brain) 50% are cancerous (Gliomas) rest 50% (20% meningioma, 15-18% pituitary adenoma, 8% shwannoma) are benign.
Success rate in safe hands is more than 95%. Complications in the form of post-operative transient neurodeficits can occur in 2-5%. Mortality in modern neurosurgery in expert hands approaches to zero.
Surgery in modern times is extremely safe. Modern equipment’s like navigation system, intraoperative monitoring techniques etc. help to improve the outcome of surgery. Besides, the neurosurgery field has advanced significantly and subspecialty neurosurgeons are the need of the day. One neurosurgeon cannot claim to be efficient in all. Jaslok hospital has such subspecialized neurosurgeons in different fields.
Average hospital stay is 7-10 days
Prognosis depends on the type of the tumor. It is excellent for benign tumor and worse for the cancerous.
To take anticonvulsants as prescribed, to follow-up regularly as advised.
WhatsApp us